Root Canal Treatment: A Step By Step Guide (video courtesy of the American Association of Endodontists)
 After profound anesthesia is confirmed, the tooth is isolated with a nitrile rubber dam (to prevent irrigants and other dental materials from getting inside the oral cavity). Next, an opening is made in the crown of the tooth. This allows access to the root canal system. A large enough opening to find all the canals within the tooth is made while also attempting to preserve as much healthy tooth structure as possible. Anatomy inside the tooth is variable. Some teeth have just one canal like most maxillary/mandibular front teeth. Premolars have 1 or 2 usually. Molars or the back teeth typically have 3 or 4 (though actual canal number can range from 1-6+). A surgical operating microscope with great illumination is used on all cases to insure proper diagnosis of each tooth’s anatomy.
After profound anesthesia is confirmed, the tooth is isolated with a nitrile rubber dam (to prevent irrigants and other dental materials from getting inside the oral cavity). Next, an opening is made in the crown of the tooth. This allows access to the root canal system. A large enough opening to find all the canals within the tooth is made while also attempting to preserve as much healthy tooth structure as possible. Anatomy inside the tooth is variable. Some teeth have just one canal like most maxillary/mandibular front teeth. Premolars have 1 or 2 usually. Molars or the back teeth typically have 3 or 4 (though actual canal number can range from 1-6+). A surgical operating microscope with great illumination is used on all cases to insure proper diagnosis of each tooth’s anatomy.
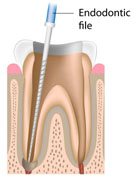 After the opening has been created by Dr. Howard and Dr. Camba, the pulp is removed from the pulp chamber and root canals. Tiny instruments (hand/rotary files) are used to clean the root canals and to shape them to a form that will be easy to fill. Irritants are used to dissolve and flush debris. If this step is not completed in one visit, medication (Calcium Hydroxide) will be placed in the canals and a temporary filling paste will be placed in the opening to protect the tooth between visits. Radiographs (X-rays) will occasionally be taken during the cleaning process to check if the instruments are cleaning near the end of the root.
After the opening has been created by Dr. Howard and Dr. Camba, the pulp is removed from the pulp chamber and root canals. Tiny instruments (hand/rotary files) are used to clean the root canals and to shape them to a form that will be easy to fill. Irritants are used to dissolve and flush debris. If this step is not completed in one visit, medication (Calcium Hydroxide) will be placed in the canals and a temporary filling paste will be placed in the opening to protect the tooth between visits. Radiographs (X-rays) will occasionally be taken during the cleaning process to check if the instruments are cleaning near the end of the root.
 When thoroughly cleaned and the tooth is primed for its final fill, the root canals are filled with a rubber-like compound called gutta percha. A cement is also used to help seal the gutta percha cones within the canals to prevent bacteria from reentering (much like bricks and mortar). We standardly take an additional step, as well, to seal the gutta percha filling by placing a flowable composite filling over the floor of the tooth to prevent possible contamination between the endodontic and the general dentist appointment. In many cases, the opening in the crown of the tooth is then sealed with a temporary filling (cotton and Cavit paste). Either upon request from your dentist or when we feel it’s appropriate, the access opening in the crown is filled with a build up restoration as pictured. Occasionally, enough tooth structure is missing to warrant use of a post to help retain the final restoration. After endodontic treatment, radiographs (X-rays) are taken to verify that cleaning and filling of the canals is close to the end of the root.
When thoroughly cleaned and the tooth is primed for its final fill, the root canals are filled with a rubber-like compound called gutta percha. A cement is also used to help seal the gutta percha cones within the canals to prevent bacteria from reentering (much like bricks and mortar). We standardly take an additional step, as well, to seal the gutta percha filling by placing a flowable composite filling over the floor of the tooth to prevent possible contamination between the endodontic and the general dentist appointment. In many cases, the opening in the crown of the tooth is then sealed with a temporary filling (cotton and Cavit paste). Either upon request from your dentist or when we feel it’s appropriate, the access opening in the crown is filled with a build up restoration as pictured. Occasionally, enough tooth structure is missing to warrant use of a post to help retain the final restoration. After endodontic treatment, radiographs (X-rays) are taken to verify that cleaning and filling of the canals is close to the end of the root.
 If a temporary filling was placed, it will be replaced by your regular dentist with a permanent filling and restoration as needed. Sometimes, only a filling (core) is required. Othertimes, a core and crown is required. Your general dentist will be responsible for the final restoration plan. A gold crown is shown for illustrative purposes, but tooth-colored crowns are often used. Crowns are required on teeth towards the back of your mouth since your mouth generates is greatest force on posterior teeth (like a nut in a nutcracker). Endodontic accesses can slightly weaken a tooth; hence, a proper filling and crown is often required. Front teeth may require restoration with a crown when not enough natural tooth structure is present but otherwise can often just be restored with a filling. Dr. Howard and Dr. Camba will discuss the requirements of your specific case after the endodontic examination and treatment planning.
If a temporary filling was placed, it will be replaced by your regular dentist with a permanent filling and restoration as needed. Sometimes, only a filling (core) is required. Othertimes, a core and crown is required. Your general dentist will be responsible for the final restoration plan. A gold crown is shown for illustrative purposes, but tooth-colored crowns are often used. Crowns are required on teeth towards the back of your mouth since your mouth generates is greatest force on posterior teeth (like a nut in a nutcracker). Endodontic accesses can slightly weaken a tooth; hence, a proper filling and crown is often required. Front teeth may require restoration with a crown when not enough natural tooth structure is present but otherwise can often just be restored with a filling. Dr. Howard and Dr. Camba will discuss the requirements of your specific case after the endodontic examination and treatment planning.
 If a build up was placed after completion of treatment, it’s important to return to your restorative dentist for completing the restoration of the tooth. Failing to return to your dentist as directed can result in fracture of the tooth, which in some instances is not repairable and tooth will have to be extracted. Other things that can happen are deterioration of the seal, decay, infection, and gum disease not to mention potentially premature loss of the tooth. You’ve already invested in maintaining the tooth, so return to your restorative dentist as soon as possible (within 1 month) for final restoration.
If a build up was placed after completion of treatment, it’s important to return to your restorative dentist for completing the restoration of the tooth. Failing to return to your dentist as directed can result in fracture of the tooth, which in some instances is not repairable and tooth will have to be extracted. Other things that can happen are deterioration of the seal, decay, infection, and gum disease not to mention potentially premature loss of the tooth. You’ve already invested in maintaining the tooth, so return to your restorative dentist as soon as possible (within 1 month) for final restoration.
There are, of course, no guarantees. Root canal or endodontic therapy has a very high degree of success, up to 90%. Teeth which can be treated near ideal have a success rate up to ninety percent! We will discuss with you the chances of success before any endodontic procedure to help you make an informed decision. If a root canal or endodontic therapy is unsuccessful or fails you still have options.
Step 1:
 After profound anesthesia is confirmed, the tooth is isolated with a nitrile rubber dam (to prevent irrigants and other dental materials from getting inside the oral cavity). Next, an opening is made in the crown of the tooth. This allows access to the root canal system. A large enough opening to find all the canals within the tooth is made while also attempting to preserve as much healthy tooth structure as possible. Anatomy inside the tooth is variable. Some teeth have just one canal like most maxillary/mandibular front teeth. Premolars have 1 or 2 usually. Molars or the back teeth typically have 3 or 4 (though actual canal number can range from 1-6+). A surgical operating microscope with great illumination is used on all cases to insure proper diagnosis of each tooth’s anatomy.
After profound anesthesia is confirmed, the tooth is isolated with a nitrile rubber dam (to prevent irrigants and other dental materials from getting inside the oral cavity). Next, an opening is made in the crown of the tooth. This allows access to the root canal system. A large enough opening to find all the canals within the tooth is made while also attempting to preserve as much healthy tooth structure as possible. Anatomy inside the tooth is variable. Some teeth have just one canal like most maxillary/mandibular front teeth. Premolars have 1 or 2 usually. Molars or the back teeth typically have 3 or 4 (though actual canal number can range from 1-6+). A surgical operating microscope with great illumination is used on all cases to insure proper diagnosis of each tooth’s anatomy.
Step 2:
 After the opening has been created by Dr. Howard and Dr. Camba, the pulp is removed from the pulp chamber and root canals. Tiny instruments (hand/rotary files) are used to clean the root canals and to shape them to a form that will be easy to fill. Irritants are used to dissolve and flush debris. If this step is not completed in one visit, medication (Calcium Hydroxide) will be placed in the canals and a temporary filling paste will be placed in the opening to protect the tooth between visits. Radiographs (X-rays) will occasionally be taken during the cleaning process to check if the instruments are cleaning near the end of the root.
After the opening has been created by Dr. Howard and Dr. Camba, the pulp is removed from the pulp chamber and root canals. Tiny instruments (hand/rotary files) are used to clean the root canals and to shape them to a form that will be easy to fill. Irritants are used to dissolve and flush debris. If this step is not completed in one visit, medication (Calcium Hydroxide) will be placed in the canals and a temporary filling paste will be placed in the opening to protect the tooth between visits. Radiographs (X-rays) will occasionally be taken during the cleaning process to check if the instruments are cleaning near the end of the root.
Step 3:
 When thoroughly cleaned and the tooth is primed for its final fill, the root canals are filled with a rubber-like compound called gutta percha. A cement is also used to help seal the gutta percha cones within the canals to prevent bacteria from reentering (much like bricks and mortar). We standardly take an additional step, as well, to seal the gutta percha filling by placing a flowable composite filling over the floor of the tooth to prevent possible contamination between the endodontic and the general dentist appointment. In many cases, the opening in the crown of the tooth is then sealed with a temporary filling (cotton and Cavit paste). Either upon request from your dentist or when we feel it’s appropriate, the access opening in the crown is filled with a build up restoration as pictured. Occasionally, enough tooth structure is missing to warrant use of a post to help retain the final restoration. After endodontic treatment, radiographs (X-rays) are taken to verify that cleaning and filling of the canals is close to the end of the root.
When thoroughly cleaned and the tooth is primed for its final fill, the root canals are filled with a rubber-like compound called gutta percha. A cement is also used to help seal the gutta percha cones within the canals to prevent bacteria from reentering (much like bricks and mortar). We standardly take an additional step, as well, to seal the gutta percha filling by placing a flowable composite filling over the floor of the tooth to prevent possible contamination between the endodontic and the general dentist appointment. In many cases, the opening in the crown of the tooth is then sealed with a temporary filling (cotton and Cavit paste). Either upon request from your dentist or when we feel it’s appropriate, the access opening in the crown is filled with a build up restoration as pictured. Occasionally, enough tooth structure is missing to warrant use of a post to help retain the final restoration. After endodontic treatment, radiographs (X-rays) are taken to verify that cleaning and filling of the canals is close to the end of the root.
Step 4:
 If a temporary filling was placed, it will be replaced by your regular dentist with a permanent filling and restoration as needed. Sometimes, only a filling (core) is required. Othertimes, a core and crown is required. Your general dentist will be responsible for the final restoration plan. A gold crown is shown for illustrative purposes, but tooth-colored crowns are often used. Crowns are required on teeth towards the back of your mouth since your mouth generates is greatest force on posterior teeth (like a nut in a nutcracker). Endodontic accesses can slightly weaken a tooth; hence, a proper filling and crown is often required. Front teeth may require restoration with a crown when not enough natural tooth structure is present but otherwise can often just be restored with a filling. Dr. Howard and Dr. Camba will discuss the requirements of your specific case after the endodontic examination and treatment planning.
If a temporary filling was placed, it will be replaced by your regular dentist with a permanent filling and restoration as needed. Sometimes, only a filling (core) is required. Othertimes, a core and crown is required. Your general dentist will be responsible for the final restoration plan. A gold crown is shown for illustrative purposes, but tooth-colored crowns are often used. Crowns are required on teeth towards the back of your mouth since your mouth generates is greatest force on posterior teeth (like a nut in a nutcracker). Endodontic accesses can slightly weaken a tooth; hence, a proper filling and crown is often required. Front teeth may require restoration with a crown when not enough natural tooth structure is present but otherwise can often just be restored with a filling. Dr. Howard and Dr. Camba will discuss the requirements of your specific case after the endodontic examination and treatment planning.
What kind of Materials are placed in the process?
The resulting space inside the center portion of your tooth is filled with a rubber like material (gutta percha) and cement (zinc oxide + eugenol) to seal the root canals in vast majority of cases. In a few special cases, the root canal space may be filled with mineral trioxide aggregate (MTA) or a plastic resin. If a filling is placed to restore an area, it will NOT contain amalgam but usually one or more of the following: composite/glass/resin ionomer (glass and organic acid +/or plastic resin), MTA (portland cement), +/or zinc oxide/eugenol.What if I have a temporary or build-up placed after treatment?
 If a build up was placed after completion of treatment, it’s important to return to your restorative dentist for completing the restoration of the tooth. Failing to return to your dentist as directed can result in fracture of the tooth, which in some instances is not repairable and tooth will have to be extracted. Other things that can happen are deterioration of the seal, decay, infection, and gum disease not to mention potentially premature loss of the tooth. You’ve already invested in maintaining the tooth, so return to your restorative dentist as soon as possible (within 1 month) for final restoration.
If a build up was placed after completion of treatment, it’s important to return to your restorative dentist for completing the restoration of the tooth. Failing to return to your dentist as directed can result in fracture of the tooth, which in some instances is not repairable and tooth will have to be extracted. Other things that can happen are deterioration of the seal, decay, infection, and gum disease not to mention potentially premature loss of the tooth. You’ve already invested in maintaining the tooth, so return to your restorative dentist as soon as possible (within 1 month) for final restoration.There are, of course, no guarantees. Root canal or endodontic therapy has a very high degree of success, up to 90%. Teeth which can be treated near ideal have a success rate up to ninety percent! We will discuss with you the chances of success before any endodontic procedure to help you make an informed decision. If a root canal or endodontic therapy is unsuccessful or fails you still have options.



